Over the past two years, there have been multiple papers and articles published pertaining to the increasing rates of syphilis in the United States. Recently I read an article “Syphilis Invades Rural America” by Lauren Weber, which led me to do a review of the subject. The referenced article speaks of the dramatic increase of syphilis infections not only in the major metropolitan areas but also in the rural communities.
In 1999, the total number of syphilis cases diagnosed nationwide was approximately 35,000. Each year since 1999, the numbers of reported syphilis cases have increased and in 2017 in excess of 101,500 cases were diagnosed. The CDC recently reported an alarming trend in the increased diagnosis of congenital syphilis from 2013 to 2017. In 2013, 362 cases of congenital syphilis were reported and by 2017, this had risen to 918 cases.
A number of problems have been identified in the diagnosis and treatment of syphilis:
- Decreased access to public health resources,
- Less practitioner experience with syphilis diagnosis,
- Reluctance to address the issue in some quarters because of conservative views toward homosexuality and non-marital sex,
- Diagnostic difficult. Syphilis has been called “the great imitator” and consequently can present differently among patients.
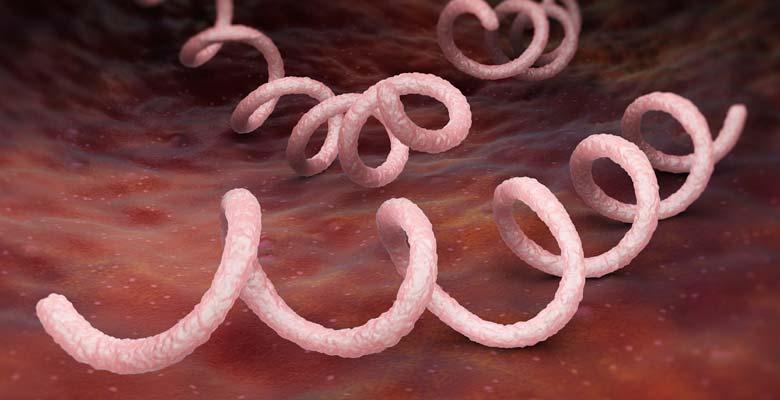
Syphilis is caused by the spirochete Treponema pallidum, the disease is divided into stages, primary, secondary, latent and tertiary, and different signs and symptoms are associated with each stage. A patient with primary syphilis will usually have a sore or sores around the site of infection be it the genital area, anus, rectum or mouth and the lesion(s) are generally painless. Secondary syphilis findings can include skin rash, lymphadenopathy and/or fever. Actually, the signs of primary and secondary syphilis might be so mild as to go unnoticed. An untreated infection will go through a latent phase potentially 10-30 years and tertiary syphilis can be associated with major medical problems affecting multiple organ systems including heart and blood vessels, brain and nervous system and the eye.
T. pallidum, the spirochete that causes syphilis, cannot be cultured. In early syphilis, the organism can be detected by dark field microscopic detection with a 70% sensitivity rate. Therefore, if dark field exam is performed and is negative, additional testing is essential so as not to miss a positive diagnosis.
If diagnosed correctly syphilis is readily treatable. It frequently is asked after treatment, “can I get syphilis again?” The answer is a resounding “yes”! In addition, after diagnosis and treatment, it is recommended that follow up laboratory testing be performed to ensure treatment has been successful.
In the next blog, I will discuss laboratory detection methods for identifying syphilis infection.
https://www.chicagotribune.com/lifestyles/health/sc-hlth-syphilis-rural-america-0508-story.html.
Also, don't forget to stay connected and join our Quality Lab Group on LinkedIn!


.png?width=261&name=2021_newest_logo_cola-footer%20(1).png)