Across the United States we saw a significant increase in the number of reported influenza cases during the last week of December. Along with the increase of diagnosed cases there was a corresponding increase in the number of hospitalizations of patients with laboratory confirmed influenza from 1.9 influenza cases/100,000 population the week before to 3.6/100,000 last week. In addition, in children younger than 5, the number of influenza confirmed hospitalizations was 10.0/100,000 and influenza infection has been responsible for 11 pediatric deaths thus far this season.
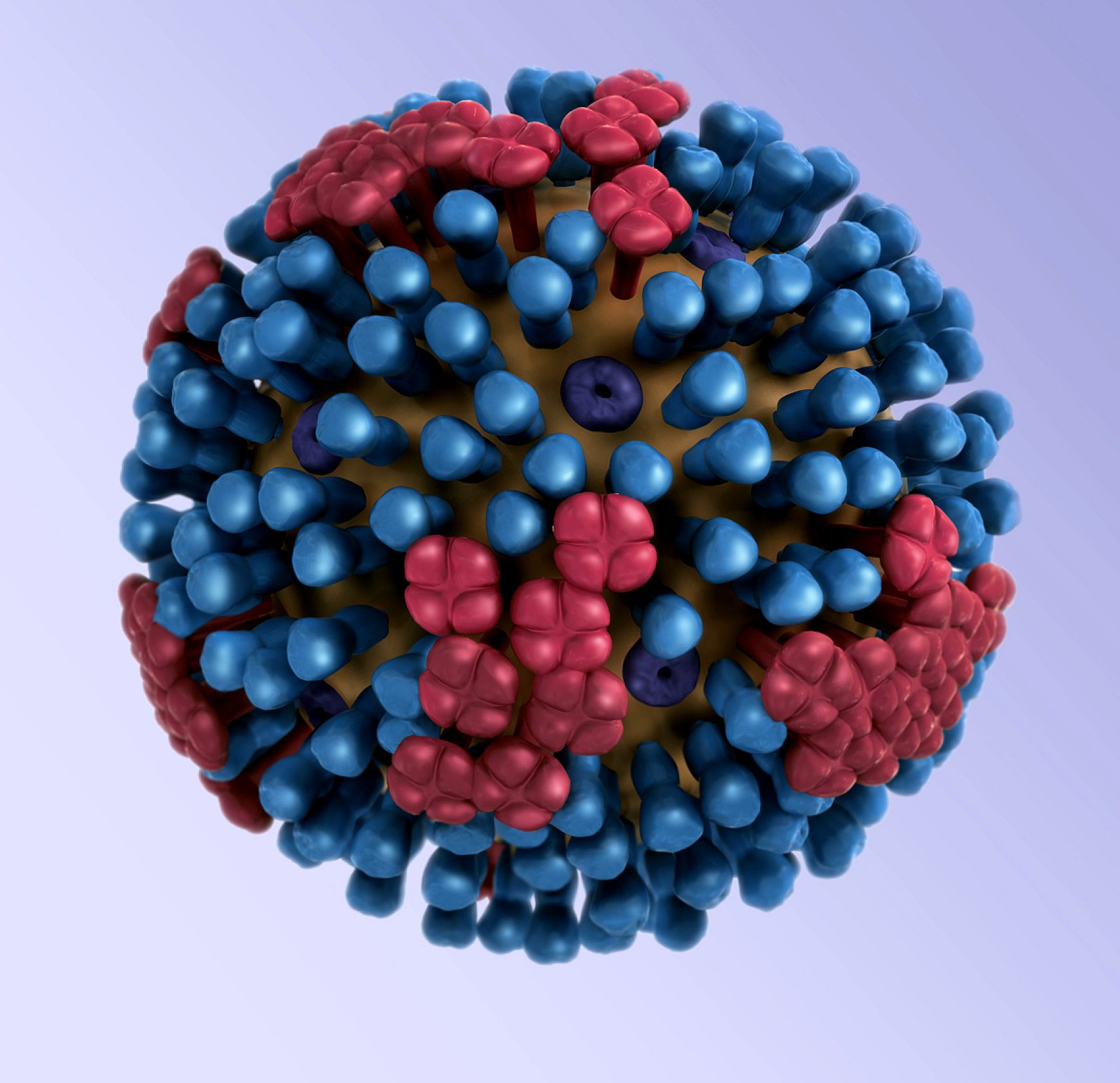
Influenza A and B viruses can cause human infection. Influenza A is divided into subtypes based on surface proteins H and N and Influenza B is grouped by lineages. Thus far in the 2018-19 influenza season, the reported infections have predominantly been Influenza A subtypes H1N1 and with a smaller number of subtype H3N2 infections reported from the Southeastern US.
Because of the low sensitivity to influenza viral detection when Class 1 immunoassays were used in testing, the FDA in late 2017 changed the classification of these devices from Class 1 to Class 2 and this led to a significant improvement in the ability of the immunoassay devices to detect the influenza virus. Overall, the sensitivity of the immunoassay test kits, which are predominantly used at the point of care, improved to greater than 70% sensitivity with the Class 2 devices. The specificity of the immunoassay devices has always been comparable to the reference method of viral culture.
At the same time the immunoassays showed this improvement, point of care molecular devices for point of care testing became available. Some of these devices are categorized as waived and many of them can be used for single patient sample testing. There are other devices that can perform influenza PCR on multiple patient samples simultaneously.
The sensitivity of the PCR methodology is comparable to the reference method of influenza viral culture and identification. The PCR technology has been favored by the clinicians because of the improved sensitivity. The turnaround time for point of care influenza testing is approximately the same for the immunoassays and the PCR testing. The shift to PCR technology does, however, add an additional financial burden. It is estimated that PCR performance may cost as much as three times the immunoassay so its use does require careful analysis of reimbursement.
However, as has been pointed out, insurers recognize that the value of the PCR technology and the accuracy of the diagnosis is being recognized by the insurers because of the reduced use of antibiotics, and more appropriate use of antiviral medication with more immediacy in patient treatment if the diagnosis is influenza. There is some anecdotal evidence that the number of subsequent hospitalizations decrease in part because of the data demonstrating up to a 25% increase in influenza diagnoses using the molecular testing.


.png?width=261&name=2021_newest_logo_cola-footer%20(1).png)